In allogeneic hematopoietic cell transplantation (allo-HCT), alloreactive T-cell responses (graft versus leukemia - GvL and graft versus host disease - GvHD) are mediated by the interaction between recipient antigens and donor lymphocytes via human leukocyte antigen (HLA) molecules.
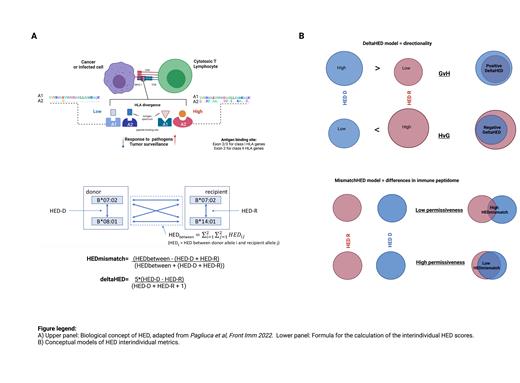
HLA evolutionary divergence (HED) is a metric recently implemented as a functional proxy for the structural variability between two homologous HLA alleles at their peptide binding sites, mirroring quantitative differences in pathogen and cancer-related immunopeptidomes ( A). 1
Here, we hypothesize that differences in and between donor and recipient HEDs at given loci may modulate the direction and the intensity of alloreactivity, informing on post-transplant outcomes. We tested this hypothesis in onco-hematologic patients undergoing allo-HCT from a single HLA-A, -B, -C, -DRB1, or -DQB1 (9/10) mismatched unrelated donor (MMUD) at EBMT centers.
We included patients with selected hematological malignancies, receiving a thymoglobulin-based T cell depletion, for whom complete clinical and HLA information was available in the EBMT database. We deployed individual locus-specific recipient/donor HED (HED-R, HED-D) metrics as previously described 1, and conceptualized two novel interindividual HED scores accounting for functional differences at the mismatched HLA loci ( A). The latter were considered as: 1) DeltaHED, quantifying the relative directional difference between HED-D and HED-R and informing on differences in immunopeptidome sizes, potentially capturing the direction and the intensity of the alloreactive response (GvH or HvG); 2) HEDmismatch, describing the HED of the mismatched locus as a proxy for the qualitative differences in immunopeptidomes between donor and recipient ( B).
Using multivariable Cox regression (cause-specific) models adjusted for relevant clinical variables, we investigated the associations of HED-R, DeltaHED and HEDmismatch, analyzed as continuous variables, with relapse free survival (RFS), overall survival (OS), non-relapse mortality (NRM), relapse and grade II-IV acute and chronic GvHD. For each outcome and in each mismatched subgroup, we built separate models for these immunogenetic parameters and checked for proportional hazards assumption (PHA). To account for multiple comparisons, only p-values <0.01 were considered significant.
Overall, 4639 adult patients, with available HLA data, received a 9/10 MMUD allo-HCT between 2010 and 2019 for acute leukemia (N=3853, 83%), myelodysplastic syndromes or myeloproliferative neoplasms (N=786, 17%). Median recipient age was 53.5 (IQR 40.2-61.9) with a male/female ratio of 1.28, whilst median donor age was 33.1 (IQR 24.5-40). Majority of patients (90%) received peripheral blood stem cells and were mismatched with their donors for locus A (33%), followed by C (21%), B (15%), DQB1 (14%) and DRB1 (6%). When analyzing the impact of HED-related parameters in each model, we observed that most recurrent associations with outcomes occurred with DRB1-related metrics. In the DRB1-mismatched subgroup (N=276), a time-varying association was found for HEDmismatch of DRB1 locus with higher HEDmismatch leading to worse RFS [HR:1.25 at t=0, (95% CI 1.1-1.42), p<0.001] and lower OS [HR:1.23 at t=0, (95%CI 1.08-1.41), p=0.002]. The strength of this associations declined over time for both endpoints (respectively RFS: HR:0.91, 95% CI 0.86-0.97, p=0.005 and OS: HR:0.93, 95% CI 0.88-0.98, p=0.013). The (directional) DeltaHED DRB1 measure instead did not display any impact on outcomes. In the same subgroup, higher HED-R in the locus C showed also a time-varying association with NRM at transplant [HR:1.89, (95% CI 1.29-2.85), p=0.002], progressively declining over time (HR:0.77, 95% CI 0.65-0.92, p=0.003). Furthermore, DRB1 HED-R modulated the probability of survival in B-mismatched subgroup, being higher scores associated with reduced OS [HR:1.03, (95%CI 1.01-1.06), p=0.009].
Here, we provide an immunogenetic benchmark to explore donor-recipient interactions in MMUD allo-HCT, demonstrating how different HLA configurations within the mismatched loci, in particular for DRB1 genes, can influence post-transplant outcomes. Given the peculiar associations observed, HED may have a role in driving early GvL effects, informing on future donor selection strategies in high-risk patients.
Disclosures
Finke:Gilead Sciences: Current holder of stock options in a privately-held company; AbbVie: Current holder of stock options in a privately-held company; Riemser: Honoraria, Research Funding, Speakers Bureau; Neovii: Honoraria, Research Funding, Speakers Bureau; Medac: Honoraria, Research Funding; Roche: Current holder of stock options in a privately-held company. Dreger:Novartis: Consultancy, Speakers Bureau; Riemser: Consultancy, Research Funding, Speakers Bureau; BMS: Consultancy, Honoraria; Gilead: Consultancy, Speakers Bureau; Beigene: Consultancy, Honoraria; AstraZeneca: Consultancy, Speakers Bureau; Abbvie: Consultancy, Speakers Bureau; Roche: Consultancy, Speakers Bureau; Miltenyi: Consultancy. Hilgendorf:Medac: Honoraria; AbbVie: Honoraria; Novartis: Consultancy, Honoraria; Takeda: Honoraria; Amgen: Honoraria; Fondatione Internationale Menarini: Honoraria; BeiGene: Honoraria; Jazz: Honoraria; Janssen: Honoraria. Peffault De Latour:Jazz Pharmaceuticals: Honoraria. Rambaldi:ABBVIE: Honoraria; Incyte: Honoraria; Roche: Honoraria; Janssen: Honoraria; Celgene-BMS: Honoraria; Novartis: Honoraria; Kite-Gilead: Honoraria; Jazz: Honoraria; Astellas: Honoraria; Pfizer: Honoraria; Agmen: Honoraria; Omeros: Honoraria. Mielke:Celgene/BMS, Novartis, Janssen, Gilead/KITE, JSMO, Pfizer: Speakers Bureau; Immunicum/Mendes, Miltenyi: Other: Participation on a Data Safety Monitoring Board or Advisory Board; SWECARNET: Other: Founder/Leadership (via my institution) ; ScientifyResearch: Other: Founder (spouse) . Merli:Sobi: Membership on an entity's Board of Directors or advisory committees; Jazz: Membership on an entity's Board of Directors or advisory committees; Miltenyi: Speakers Bureau; Amgen: Speakers Bureau.